Relationship Between Sleep and Antidepressants
Antidepressants and sleep have a complicated and nuanced relationship. Although these drugs are very helpful in treating mood disorders, they can also affect the general sleep-wake cycles, as well as the quantity and pattern of sleep. In order to effectively navigate treatment and support optimum sleep hygiene, healthcare providers and patients must have a thorough understanding of the dynamics of antidepressants on sleep. This article examines antidepressant effects on sleep, frequent side effects linked to sleep, methods for treating sleep problems, and factors to take into account while attempting to strike the ideal balance between mental health therapy and sleep quality.
Antidepressants' Effects on Sleep
Neurotransmitters and the Architecture of Sleep
Rapid eye movement (REM) and non-rapid eye movement (NREM) sleep are two of the stages of the dynamic process that is sleep. Serotonin, norepinephrine, and dopamine are examples of neurotransmitters that are crucial for controlling sleep-wake cycles and sleep architecture. Antidepressants that target these neurotransmitter systems have the potential to impact the duration, quality, and phases of sleep.
Common Side Effects of Sleep
Insomnia: When taking certain antidepressants, especially SSRIs and SNRIs, some people first get insomnia. During the first few weeks of treatment, it's possible to have trouble falling or staying asleep, but as the body becomes used to the medicine, these issues may get better.
During the day: Conversely, drowsiness or sedation during the day can be brought on by several antidepressants, including TCAs and other typical antidepressants, which can impair alertness and functioning during the day.
Changes in REM Sleep: Certain antidepressants may cause REM sleep suppression or changes in the architecture of REM sleep, which can result in vivid dreams, nightmares, or adjustments to the intensity and memory of dreams.
Techniques to Handle Sleep Disturbances
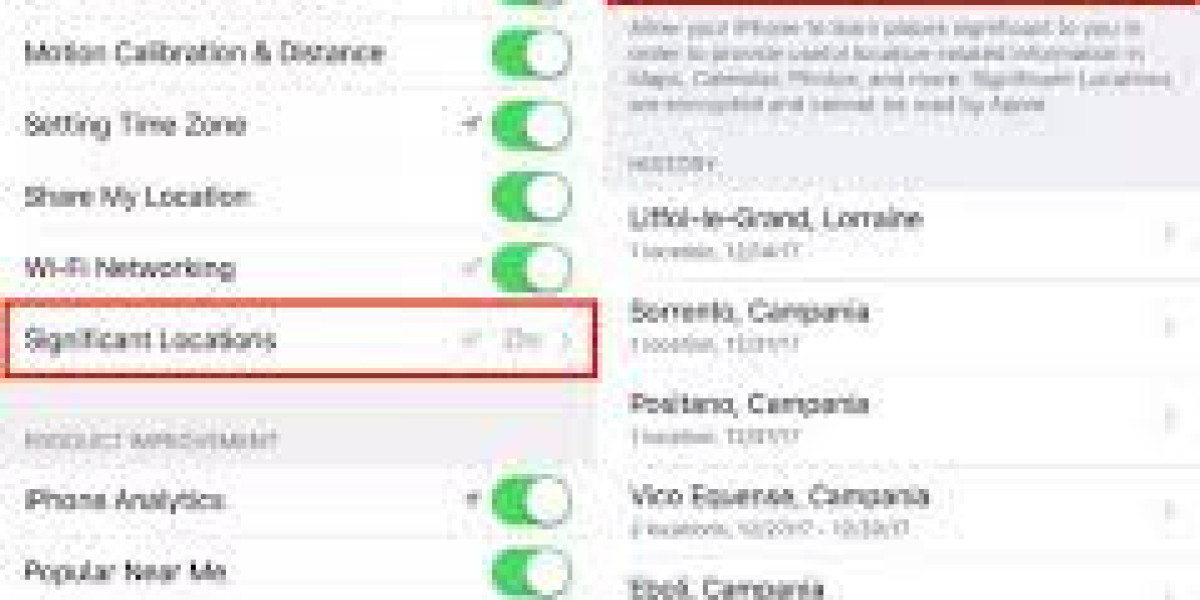
When to Take Medication
Discussing the time of antidepressant use with a healthcare professional can help reduce adverse effects linked to sleep. Optimizing sleep-wake cycles can be achieved by taking drugs in the morning or early afternoon (for sedatives) or by changing dosages closer to bedtime (for agents causing initial insomnia).
Changes in Lifestyle to Improve Sleep
Suitable Sleep Position: Better sleep quality can be encouraged by establishing a regular sleep schedule, developing a calming bedtime ritual, and optimizing the sleep environment (e.g., lowering noise levels, regulating room temperature).
Limiting the Input:
You can make falling asleep easier by avoiding stimulating activities right before bed, caffeine, and nicotine.
Techniques for Relaxation and Mindfulness
Reduce tension and encourage sleep-promoting relaxation before bedtime by engaging in progressive muscle relaxation, deep breathing techniques, or mindfulness meditation.
Extra Interventions
Additional therapies may be helpful for those whose sleep difficulties persist even after they have changed their lifestyle and taken medicine as prescribed:
Sleep Aids: Under medical supervision, the short-term use of over-the-counter or prescription sleep aids may assist regulate sleep patterns. However, because of the possibility of reliance and rebound insomnia, they should only be used sparingly.
Insomnia Treatment with Cognitive Behavioral Therapy (CBT-I):
With an emphasis on behavioral interventions, cognitive restructuring, and sleep education, CBT-I is an organized, research-based therapy that treats insomnia and enhances sleep quality without the need for medication.
Customized Approach and Care Coordination with Medical Professionals
In order to treat sleep issues related to antidepressant therapy, the patient-provider relationship must be open. Treatment programs can be customized by providers according to each patient's unique medication reaction, sleep habits, and general state of mental health. Frequent check-ups make it possible to track changes in the quality of sleep, modify drug schedules as necessary, and investigate different approaches to sleep management.
Entire Mental Health Evaluation
Given the reciprocal relationship between sleep and mental health, thorough evaluations that take into account stressors, lifestyle choices, mood symptoms, and sleep habits are essential. Effectively treating underlying mental health issues can enhance sleep quality indirectly, and vice versa.
In conclusion, finding a balance to promote holistic health
Achieving the ideal balance in the interaction between antidepressants and sleep is essential for fostering overall wellbeing. Antidepressants are essential for treating mood disorders, but their effects on sleep emphasize the need for individualized care plans, lifestyle changes, and continuous observation. Effective management of sleep disruptions can be achieved by fostering collaboration among patients, healthcare professionals, and sleep specialists to enhance mental health results. Adopting a holistic strategy that gives equal weight to sleep hygiene and mental health promotes overall wellness and improves the quality of life for those who are dealing with mental health issues.