Pharmacy Benefit Management (PBM) is defined as companies that act as an intermediary between insurance companies, manufacturers, and pharmacies. Pharmacy benefit management helps to provide medical services and medications to employers at a low cost. The PBM managers negotiate with the drug makers to secure a discount on drug prices and pass the savings to insurers.
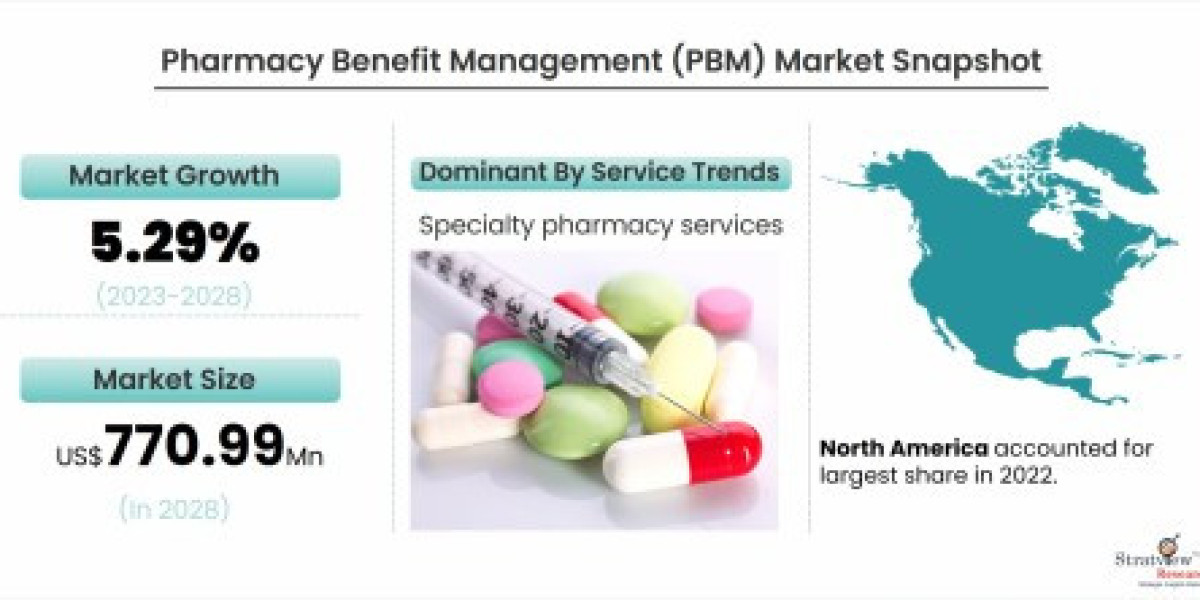
"The global pharmacy benefit management (PBM) market is estimated to grow from USD 563.96 Million in 2022 to USD 770.99 Million by 2028 at a CAGR of 5.29% during the forecast period".
The Pharmacy Benefit Management (PBM) market plays a crucial role in the healthcare ecosystem by managing prescription drug programs on behalf of health insurers, employers, and government programs. PBMs act as intermediaries between insurers, pharmaceutical manufacturers, and pharmacies, negotiating drug prices and managing formularies to optimize healthcare costs.
Key Drivers of Growth
One of the main factors driving the growth of the PBM market is the rising cost of prescription drugs. With healthcare expenses on the rise, employers and insurers are increasingly relying on PBMs to control medication costs through formulary management, rebate negotiations, and cost-sharing strategies. The growing number of people with chronic diseases that require long-term medication has also spurred demand for PBM services. Additionally, the aging population has led to an increase in prescription drug utilization, further bolstering the market.
Another significant driver is the increasing consolidation in the healthcare industry. Large health insurers have begun acquiring or merging with PBMs to create integrated systems that better control costs, improve care coordination, and enhance service efficiency. For example, CVS Health’s acquisition of Aetna and Cigna’s merger with Express Scripts have set the stage for the rise of such integrated healthcare models.
Challenges Facing the PBM Market
Despite its growth, the PBM market faces challenges such as regulatory scrutiny and calls for greater transparency. Critics argue that the complex rebate structures used by PBMs can contribute to higher drug costs, rather than reducing them. Regulatory authorities are now pushing for more transparency in pricing and contract practices, which could reshape the market's dynamics.
Future Outlook
As healthcare costs continue to rise, the PBM market is expected to grow steadily. Technological advancements, such as the use of artificial intelligence to predict drug utilization patterns and optimize formularies, are also expected to play a significant role in the future of PBM services. With increasing pressure for transparency and cost control, PBMs will remain a key player in the evolving healthcare landscape.
To learn more about the market dynamics, Register Here: https://www.stratviewresearch.com/Request-Sample/1796/pharmacy-benefit-management-(PBM)-market.html#form